The Ultimate TMS Treatment Guide by TMS Treatment Florida
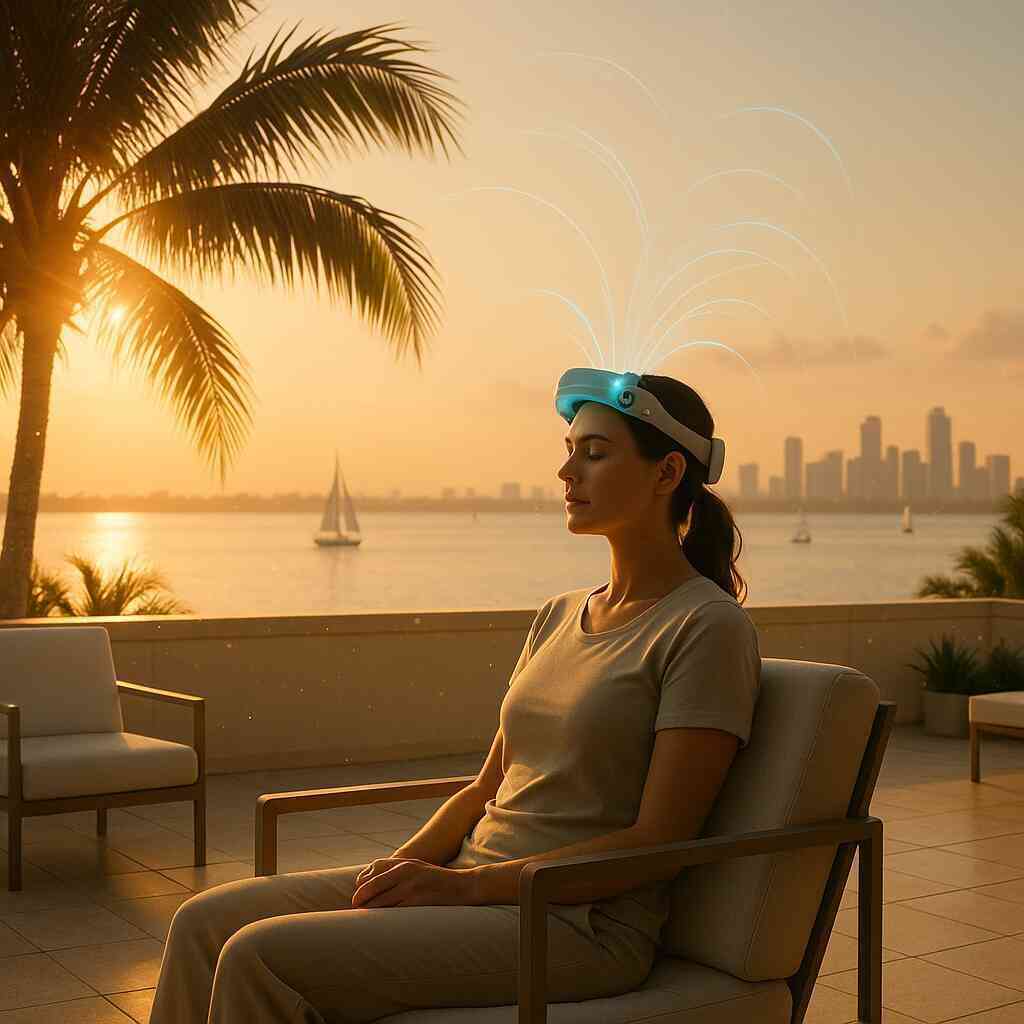
Unlocking Brighter Horizons: How TMS Treatment Florida Redefines Mental Wellness
The evolution of non invasive brain stimulation therapy
The story of brain stimulation therapy spans decades, yet its modern chapter feels revolutionary. Early scientists explored electricity to calm psychiatric turbulence, but tolerability lagged behind promise. Today, Transcranial Magnetic Stimulation, or TMS, achieves precision without anesthesia or memory disruption. This non-invasive brain stimulation therapy uses focused magnetic pulses to gently awaken dormant neural circuits. Because it respects the brain’s complexity, it preserves personality while releasing people from oppressive mood disorders.
Florida clinicians have embraced this evolution, integrating cutting edge mental health technology into welcoming outpatient environments. Patients who once cycled through medications now discover reliable depression relief with TMS delivered in brief sessions. Our clinic’s comprehensive TMS care in Florida model blends rigor with warmth, keeping outcomes and comfort perfectly aligned. As coils deliver rhythmic pulses, neuroplasticity blooms, strengthening mood regulating networks that medication alone could not reach. Such progress underscores why a modern Transcranial Magnetic Stimulation guide must feature the Sunshine State.
Why TMS therapy Florida is gaining momentum
Across Florida’s diverse communities, demand for non drug pathways grows louder every season. Residents juggling careers, caregiving, and coastal commutes crave treatments that work without sidelining productivity. TMS therapy Florida fulfills that need because sessions finish before a lunch hour ends. Unlike systemic medications, magnetic pulses stay localized, sparing digestion, libido, and sleep architecture. Word of mouth travels quickly when side effects remain minimal and mood lifts feel authentic.
Healthcare analytics confirm the trend. Utilization rates of advanced TMS treatment options have doubled among Floridians diagnosed with anxiety disorders. Clinics tailor anxiety management TMS protocol settings to each cortex, lowering fear circuitry activation without sedation. Similarly, targeted coils achieve meaningful OCD symptom reduction TMS clinicians once only imagined. For individuals cycling between highs and lows, bipolar disorder TMS support offers stability without metabolic burdens.
From stigma to science a new era for mood disorder treatment innovations
Historical misconceptions painted brain stimulation as extreme, yet modern evidence dismantles lingering stigma. Peer reviewed trials now compare TMS vs medication outcomes head to head. Results consistently reveal equivalent or superior remission rates with far fewer systemic adverse events. Imaging studies illustrate TMS neuroplasticity benefits, showing densified synaptic connections in mood regulation hubs. Such visual proof transforms abstract science into tangible hope for families previously skeptical.
Florida research centers also pioneer combined protocols, pairing magnetic pulses with rapid recovery depression therapies like low dose ketamine. This integrative model recognizes that complex neurobiology rarely yields to one input alone. When TMS primes cortical neurons, subsequent pharmacologic or psychotherapeutic cues embed more deeply, shortening overall recovery timelines. The outcome represents a decisive cultural shift where science, compassion, and innovation coalesce for unmatched mood disorder treatment innovations. Every success story chips away further at outdated stereotypes, inviting broader access across the state.
Inside the Magnetic Pulse: Understanding the Mechanics and Benefits
TMS neuroplasticity benefits demystified
Transcranial Magnetic Stimulation awakens sluggish neural pathways through gentle, rhythmic pulses that mirror natural brain oscillations. This non-invasive brain stimulation therapy sparks long-term potentiation, a process where new synapses strengthen mood circuits. As connections multiply, patients describe authentic energy returning, not the artificial lift sometimes reported with pharmaceuticals. Clinicians prize these TMS neuroplasticity benefits because they endure, supporting depression relief with TMS months after treatment ends. Curious readers can explore the underlying mechanics behind magnetic neurotherapy to appreciate how physics translates into profound emotional change.
Scientific imaging illustrates cortical growth after each session, confirming that electrochemical resilience is no longer theoretical. Repeated studies show heightened activity in the dorsolateral prefrontal cortex, the region dimmed by chronic sadness. Because stimulation stays localized, memory, speech, and creativity remain unharmed. Such precision showcases the cutting-edge mental health technology powering this Transcranial Magnetic Stimulation guide. Ultimately, patients gain hope through tangible proof rather than abstract promises.
Advanced TMS treatment options compared to medication
Traditional antidepressants flood the entire body, inviting metabolic, gastrointestinal, and sexual side effects many Floridians cannot tolerate. In contrast, advanced TMS treatment options concentrate energy only where mood regulation originates, sparing the rest of the system. This targeted strategy yields remission rates rivaling first-line medicines, yet with far fewer discontinuations. A fair TMS vs medication comparison also highlights rapid onset; improvements often surface within weeks rather than months. When urgency matters, neurostimulation’s fast trajectory can feel lifesaving.
Innovation does not stop at standard high-frequency protocols. Theta-burst, accelerated schedules, and deep-coil approaches now customize pulse patterns for stubborn symptoms. These mood disorder treatment innovations adapt intensity, coil angle, and frequency to individual neuroanatomy. Because each brain processes signals differently, flexible programming matters more than a one-size pill. This suite of options proves why TMS therapy Florida continues gaining respected clinical ground.
Anxiety management TMS protocol and beyond
Anxiety often hides beneath depression, yet it responds uniquely to magnetic modulation. A dedicated anxiety management TMS protocol targets right prefrontal circuits implicated in hypervigilance and worry. Patients report calmer breathing, steadier focus, and fewer racing thoughts after several sessions. Unlike benzodiazepines, stimulation avoids sedation, allowing employees and students to sustain productivity. These outcomes make anxiety management TMS protocol strategies increasingly popular throughout beachside and urban clinics alike.
Beyond generalized anxiety, specialized coil placements address OCD symptom reduction TMS research now validates. By modulating supplementary motor areas, intrusive rituals gradually loosen their grip. Simultaneously, exploring TMS for anxiety near South Florida communities inspires open dialogue and earlier intervention. The same technology assists trauma survivors when paired with psychotherapy, extending relief from the amygdala’s fear memory loops. Safe versatility keeps clinicians reaching for TMS first, not last.
Personalized TMS care plans for complex mood disorders
Depression rarely travels alone; bipolar swings, chronic pain, or attention deficits often complicate recovery. Personalized TMS care plans layer stimulation parameters around each diagnostic nuance, ensuring no condition gets neglected. For manic-depressive patterns, bipolar disorder TMS support focuses on stabilizing mood without triggering hypomania. Low-frequency right-sided pulses gently temper elevated states, while high-frequency left-sided pulses combat sinking periods. This dual approach offers harmony that conventional medications sometimes disturb.
Customization extends to coil design, session count, and real-time motor threshold monitoring. Clinicians adjust settings as cortical excitability evolves, preventing plateau and maximizing neuroplastic change. Family input, daily mood logs, and wearable sleep trackers refine protocols further. The result is a living treatment blueprint rather than a static schedule. Such responsiveness epitomizes personalized TMS care plans and cements Florida’s leadership in precision psychiatry.
Evidence based mood disorder treatments powering hope
Data remains the backbone of medical trust, and TMS delivers a towering evidence stack. Meta-analyses across thousands of participants confirm significant response rates, even in medication-resistant cases. These evidence-based mood disorder treatments empower practitioners to recommend stimulation with conviction, not speculation. Patient testimonials add another layer, with many TMS success stories Florida families eagerly share at community forums. Numbers and narratives together cultivate hope where despair once dominated.
Forward-thinking clinics also combine magnetic pulses with rapid recovery depression therapies like ketamine infusion. This ketamine treatment synergy with TMS accelerates relief by engaging glutamate pathways alongside cortical modulation. Early trials reveal greater remission durability when therapies unite rather than compete. By exploring ketamine clinic Florida insights, providers craft holistic mental wellness strategies that respect neurobiology’s complexity. A future where mood disorders lose their grip feels closer than ever.

Designing Your Journey From Consultation to Lasting Change
TMS patient eligibility checklist and expectations
Every successful treatment begins with a clear TMS patient eligibility checklist at hand. Our clinicians review medical history, current medications, and any implanted devices during the consultation. They confirm diagnoses such as major depression, anxiety, OCD, or bipolar disorder meet evidence-based criteria. Patients who failed two antidepressant trials often benefit most from non-invasive brain stimulation therapy. During orientation, we address common questions on non invasive brain stimulation to build transparent trust. Expectations become realistic when individuals learn that improvement typically appears gradually over several weeks. We emphasize that personality remains untouched while mood circuits gain healthier flexibility. This clarity empowers families to pursue depression relief with TMS confidently and collaboratively.
Beyond diagnosis, physical health factors influence eligibility for advanced TMS treatment options. Uncontrolled seizures, recent brain injury, or ferromagnetic cranial implants present contraindications requiring alternative plans. Pregnancy, meanwhile, rarely prevents therapy, although obstetric coordination ensures complete safety. Our team also screens for severe substance misuse that might cloud symptom tracking. Because personalized TMS care plans adapt stimulation intensity, motor threshold testing determines safe dosage. Patients practicing mindful living, regular sleep, and balanced nutrition typically demonstrate heightened TMS neuroplasticity benefits. Finally, commitment to attend weekday sessions underpins treatment success by sustaining cortical momentum. Understanding these expectations removes surprises and sets the stage for measurable mental wellness progress.
Prepare for first TMS session like a pro
Preparation transforms a first appointment from uncertain to empowering. Start by wearing comfortable clothing without metallic accessories that could interfere with magnetic fields. Eat a balanced breakfast because steady blood sugar supports focus during mapping procedures. Bring a list of medications, previous therapies, and allergy notes for rapid review. Arriving fifteen minutes early allows relaxation, breathing exercises, and final questions. During scalp measurement, technicians locate the dorsolateral prefrontal cortex, tailoring coil placement to your anatomy. You will feel gentle tapping sensations, not painful shocks, as the motor threshold gets established. A personal belief in change boosts response, so visualize post-treatment victories while pulses start.
Many patients compare the initial visit to a dental cleaning in duration and intensity. Noise-canceling headphones and mood playlists reduce coil clicking awareness. Some bring inspirational podcasts to reinforce holistic mental wellness strategies. Hydration matters, so carry a water bottle and sip between pulse trains if advised. Communicate any discomfort immediately; clinicians adjust seating angles or cushion placement promptly. Because TMS therapy Florida emphasizes individualized care, technicians note your feedback for future sessions. After treatment, schedule follow-up visits before leaving to maintain consistent cortical engagement. Finally, reward yourself with a healthy lunch afterward, anchoring positive associations with each visit.
Daily life during a TMS course sustaining balance
A standard course involves weekday visits, yet life outside the clinic continues gracefully. Clients usually drive themselves, return to work, or attend classes immediately after sessions. To sustain balance, carve ten daily minutes for mindfulness that amplifies neuroplastic gains. Regular aerobic exercise enhances cerebral blood flow, complementing cutting-edge mental health technology benefits. Prioritize consistent sleep, because overnight consolidation locks in mood circuit improvements. Avoid excessive alcohol, as it dampens synaptic potentiation and blunts progress. Support systems matter; share milestones with friends to reinforce emerging optimism. Document shifts in energy, appetite, and concentration using a mood tracking app daily.
Nutrition choices influence neurotransmitter production throughout the TMS course. Include omega-3 rich foods, leafy greens, and lean proteins for resilient brain chemistry. Stay hydrated, because adequate fluids facilitate neuronal metabolism and waste clearance. Strategically schedule demanding tasks soon after sessions when focus typically peaks. Leverage growing motivation to engage in therapy homework or creative projects. If emotional turbulence arises, remind yourself that neurocircuitry recalibration sometimes surfaces uncomfortable memories. Reach out to clinicians quickly; adjustments to frequency or supportive counseling provide relief. Celebrating small victories weekly sustains momentum until the final pulse completes the protocol.
Side effects of TMS explained with clarity
Transparency about side effects of TMS explains fosters trust and reduces anxiety. Most participants experience only mild scalp tenderness near the stimulation site. Discomfort usually fades within days as tissue acclimates to rhythmic pulses. Occasional headaches respond well to over-the-counter analgesics and hydration. Unlike systemic medications, TMS spares digestion, sexual function, and weight regulation. No memory loss occurs, distinguishing it from historical electroconvulsive procedures. Seizure risk remains exceptionally rare, comparable to everyday office computer use. Clinics maintain emergency protocols regardless, exemplifying rigorous patient safety culture.
Some patients notice transient lightheadedness immediately post-session. Sitting briefly and deep breathing restores equilibrium quickly. Auditory tolerance improves when foam earplugs mute coil clicking noise. Mood activation may cause temporary emotional sensitivity during early weeks. Therapists normalize this experience, explaining neuroplastic transitions underlie the feelings. Reporting symptoms promptly allows parameter refinements that prevent escalation. Overall, studies confirm TMS vs medication comparison favors stimulation for tolerability. Clear education transforms potential worries into confident participation throughout the series.
Combining TMS and psychotherapy for rapid recovery
Magnetic pulses prime neuronal networks, yet cognitive skills anchor lasting change. Therefore, combining TMS and psychotherapy multiplies therapeutic power for rapid recovery depression therapies. Cognitive behavioral sessions scheduled shortly after stimulation leverage heightened cortical receptivity. Patients integrate new thought patterns more quickly, reducing relapse probability. Mindfulness training complements anxiety management TMS protocol by teaching present-focused breathing. Exposure rituals shrink faster when OCD symptom reduction TMS dampens intrusive urges. For bipolar disorder TMS support, psychoeducation helps identify early mood shift signals. The dual strategy aligns with holistic mental wellness strategies championed across Florida.
Clinicians coordinate session timing, often reserving therapy rooms adjacent to stimulation suites. This logistical convenience reduces travel fatigue and maintains motivational momentum. Insurance coverage for combined services frequently requires clear documentation of medical necessity. Our administrative team liaises with carriers, preventing bureaucratic delays. Regular interdisciplinary meetings ensure treatment adjustments reflect evolving clinical progress. Patients feel heard, observed, and championed by a unified care team. Such coordinated attention fosters TMS success stories Florida residents enthusiastically share. Ultimately, integration shows science and empathy can coexist seamlessly within modern psychiatry.
Ketamine treatment synergy with TMS unlocking resistant depression relief
Some depressive episodes resist even advanced TMS treatment options and multiple medication trials. Introducing ketamine treatment Florida protocols can shift neurochemical landscapes quickly. Low-dose intravenous or intranasal ketamine boosts glutamate signaling, opening synaptic growth windows. Delivering TMS during that window reinforces newly sprouted pathways, forging durable mood resilience. Research labels this partnership ketamine treatment synergy with TMS, a promising frontier. Patients often report rapid lift within days, shortening emotional suffering substantially. Ketamine therapy in Florida clinics follows strict monitoring, ensuring cardiovascular and dissociative safety. Combining protocols remains voluntary, respecting individual comfort and cultural perspectives.
Our specialists educate clients on potential transient dizziness or mild perceptual shifts after ketamine. Quiet recovery rooms and supportive staff normalize the experience until clarity returns. Regular liver function assessments uphold medical integrity throughout the series. We collaborate with ketamine clinic Florida insights to refine dosing frameworks continually. Patients from coastal communities access ketamine in South Florida resources for convenient follow-ups. When combined, both modalities showcase mood disorder treatment innovations once considered futuristic. Long-term outcomes after TMS enhanced by ketamine appear especially favorable in recent registries. As evidence grows, insurance payers increasingly recognize the cost effectiveness of this synergy.
Insurance coverage for TMS therapy navigating logistics
Financial clarity reduces stress, enabling clients to focus on healing. Most major insurers now classify TMS as medically necessary for treatment-resistant depression. Carriers usually require documentation of two failed pharmacologic trials and licensed psychiatric evaluation. Our coordinators assemble those records, submit them, and track approvals diligently. Appeals teams step in immediately if denials surface, armed with robust evidence-based mood disorder treatments. For anxiety, OCD, or bipolar indications, preauthorization criteria vary across provider networks. We guide families through forms, peer reviews, and out-of-pocket estimations transparently. Understanding insurance coverage for TMS therapy early prevents unpleasant surprises down the road.
Public programs like Medicare also reimburse when specific clinical benchmarks are met. Veteran benefits often include dedicated neurostimulation allocations, reflecting military mental health priorities. Payment plans remain available for individuals awaiting coverage decisions or choosing elective enhancements. Flexible spending accounts and health savings accounts may offset copayments or deductibles. We provide itemized receipts formatted for seamless reimbursement submission. Transparent cost communication aligns with our commitment to trustworthiness and community stewardship. By removing financial confusion, we keep the healing journey emotionally focused and forward looking. Navigating logistics smoothly reinforces confidence, encouraging adherence until remission stabilizes.
Choosing a TMS provider in Florida what matters most
Selecting a clinic feels daunting amid Florida’s expanding landscape of neurostimulation centers. Prioritize expertise, beginning with board-certified psychiatrists supervising every session. Advanced TMS services in Miami Dade County demonstrate how regional excellence raises care standards. Equally, cutting edge TMS therapy near Broward County offers convenient access for commuters. Evaluate whether clinics maintain multiple coil types to support personalized TMS care plans. Ask about onsite outcome tracking, because data transparency signals accountability. Tour facilities to confirm calming aesthetics, private suites, and disability accommodations. Finally, inquire about crisis protocols, showing dedication to comprehensive safety.
Human connection matters as much as machinery. Seek compassionate staff who listen, explain, and celebrate small milestones. Look for therapists ready to integrate sessions, solidifying change beyond the coil. An expert transcranial magnetic stimulation team in Florida coordinates multidisciplinary voices seamlessly. Verify that providers discuss long-term maintenance, not just acute intervention. Ask about community resources, support groups, and telehealth check-ins after completion. Positive reviews, published outcomes, and word-of-mouth recommendations strengthen credibility further. When qualities align, choosing becomes easy, and recovery momentum accelerates confidently.
Future Focused Healing Sustaining Results and Expanding Possibilities
Post treatment TMS maintenance strategies
Finishing the acute series is a milestone, yet neuroplastic change continues for months. Clinicians often recommend scheduled booster sessions to refresh cortical circuits when stress peaks. These brief appointments resemble the original protocol but occur less frequently, preserving gains without disruption. Patients who pair boosters with consistent sleep, nutrition, and exercise report steadier mood trajectories. Tracking symptoms through a digital diary helps teams time boosters proactively instead of reactively.
Lifestyle alignment further secures post-treatment stability. Daily mindfulness practice calms limbic reactivity, reinforcing the balanced prefrontal activity sparked by TMS. Moderate aerobic activity three times weekly increases hippocampal growth factors, enhancing resilience. Reducing alcohol, especially during high-pressure seasons, protects synaptic health and decision clarity. Support groups offer social accountability, reminding graduates they are never alone in maintenance. When combined, these habits transform short-term remission into long-term flourishing.
Long term outcomes after TMS what the data reveal
Large follow-up studies track participants for several years after completion. Findings consistently show over half remain in full remission twelve months later, even without additional medication changes. Those who needed intermittent boosters maintained comparable success, underscoring the therapy’s durability. Neuroimaging confirms persistent activation in dorsal prefrontal regions, suggesting structural adaptation rather than temporary excitement. Such objective evidence strengthens confidence among skeptics who once doubted stimulation longevity.
Researchers also observe cascading benefits beyond mood. Many participants report improved cognitive flexibility, enabling quicker problem solving at work. Enhanced sleep architecture appears in polysomnographic recordings, indicating deeper restorative cycles. Anxiety scores often continue declining, likely because worry circuits receive less amygdala input over time. Importantly, serious adverse events remain rare in extended tracking. Together, these metrics paint a hopeful picture for anyone considering a first course today.
TMS success stories Florida inspiring next steps
Across the state, personal narratives breathe life into statistics. A teacher from Tampa regained classroom passion after decades of depressive fog, crediting morning sessions for lighting creative sparks. A retired veteran in Jacksonville celebrated hiking again because anxiety no longer hijacked breathing on trails. Such victories, echoed in countless clinics, prove that perseverance coupled with skilled guidance yields transformation.
Clinicians compile these journeys as motivational resources for new patients. Hearing peers describe the first genuine laugh after years of numbness fosters immediate connection. Families also gain encouragement when they learn how relationships healed once intrusive symptoms eased. These success stories ignite hope for continuous growth, inspiring graduates to mentor incoming participants. Community momentum ultimately propels mental wellness beyond clinical walls.
Ketamine clinic Florida insights for comprehensive care
For individuals facing entrenched, treatment-resistant depression, combining modalities can spark breakthroughs. Low-dose ketamine rapidly amplifies glutamatergic signaling, opening a window where TMS can sculpt enduring pathways. Medical teams coordinate infusion timing, monitor vitals, and adjust coil parameters to maximize synergy. Integration remains personalized, respecting biological variability and individual comfort levels. Early registries reveal accelerated relief and fewer relapses when both tools collaborate thoughtfully.
Patients exploring this path often request reliable information channels. Our clinicians recommend reviewing vetted ketamine therapy resources in Florida to understand protocols, eligibility, and safety measures. Transparent education reduces apprehension about dissociative experiences or cardiovascular monitoring. Financial counselors help navigate insurance language, as combined care increasingly gains coverage. When structured responsibly, ketamine-TMS partnerships broaden the therapeutic horizon for those who previously felt stuck.
Embracing holistic mental wellness strategies beyond the clinic
Sustainable recovery blossoms when medical interventions meet intentional daily living. Nutrient-dense meals rich in omega-3 fatty acids nourish membrane fluidity and neurotransmitter balance. Consistent circadian routines anchor hormones, reducing vulnerability to mood swings. Mindful breathing before meetings interrupts catastrophic thinking loops that once dominated. Creative outlets-music, gardening, or painting-channel emotional energy into restorative expression. Each habit reinforces neural pathways strengthened during treatment.
Environmental and technological supports extend these gains. Sunlight exposure during morning walks synchronizes internal clocks, boosting serotonin naturally. Blue-light filters on devices protect melatonin release, securing restorative sleep. Mobile apps offer guided meditations, mood tracking, and peer forums, ensuring accountability between appointments. Regular check-ins with primary therapists maintain therapeutic momentum as new life chapters unfold. By weaving these strategies together, graduates craft a resilient lifestyle where wellness becomes the norm rather than the exception.
 Frequently Asked Questions
Frequently Asked Questions
Question: What makes TMS Treatment Florida’s personalized TMS care plans different from other clinics in the state?
Answer: Our team builds every plan from the ground up, starting with a thorough TMS patient eligibility checklist, motor-threshold mapping, and real-time data tracking. Because we keep multiple coil types and advanced TMS treatment options in house-high-frequency, theta-burst, and deep-coil-we can fine-tune pulse patterns for depression relief with TMS, anxiety management, OCD symptom reduction, or bipolar disorder TMS support without a one-size-fits-all mentality. The result is a truly personalized TMS care plan that adapts to your brain’s evolving neuroplasticity benefits while preserving comfort and convenience.
Question: How does your anxiety management TMS protocol work, and what kind of results do patients generally experience?
Answer: Our protocol targets the right dorsolateral prefrontal cortex-an area that drives hypervigilance and racing thoughts-using low-frequency stimulation to calm overactivity. Most patients begin noticing steadier focus and fewer panic spikes within two to three weeks. Because TMS is a non-invasive brain stimulation therapy, you can return to work or class immediately after each session, with minimal side effects of TMS explained clearly up front. Long-term outcomes after TMS show sustained reductions in GAD-7 anxiety scores, and many clients share their TMS success stories Florida-wide, highlighting improved sleep and productivity.
Question: In The Ultimate TMS Treatment Guide by TMS Treatment Florida, you mention ketamine treatment synergy with TMS. Who qualifies for this combined approach, and how does it enhance rapid recovery depression therapies?
Answer: We consider the ketamine clinic Florida insights for anyone who has tried at least two antidepressants and one full course of standard TMS without adequate relief. Low-dose ketamine quickly boosts glutamate activity, opening a neuroplastic window that our coils can then consolidate. This ketamine treatment synergy with TMS often accelerates mood lift from weeks to days, making it ideal for treatment-resistant depression. Safety is paramount: vitals are monitored during each ketamine therapy in Florida session, and board-certified psychiatrists oversee the integrated protocol.
Question: What side effects should I realistically expect from your Transcranial Magnetic Stimulation guide, and how do you keep treatments safe?
Answer: The most common effects are mild scalp tenderness or a brief tension-type headache, typically fading after a day and managed with hydration or OTC analgesics. Unlike medication, TMS leaves digestion, libido, and cognition untouched. Seizure risk is extremely low-comparable to daily computer use-and our clinic follows rigorous emergency protocols regardless. You will always wear ear protection to soften coil clicks, and technicians adjust intensity immediately if discomfort arises. By offering honest side effects of TMS explained before the first pulse, we build the trust you deserve.
Question: Will my insurance cover TMS therapy, and how does TMS Treatment Florida help me navigate the paperwork?
Answer: Most major insurers-including Medicare-recognize TMS as an evidence-based mood disorder treatment, especially after two failed medication trials. Our coordinators assemble medical records, submit prior-authorizations, and track approvals, so you avoid bureaucratic headaches. If a carrier denies coverage, we immediately file appeals backed by peer-reviewed data that highlight the favorable TMS vs medication comparison. We also offer flexible payment plans, accept HSA/FSA funds, and provide itemized receipts for reimbursement. Clear communication about insurance coverage for TMS therapy ensures finances never derail your path to mental wellness.


